Longtime activist, Victory Fund co-founder David Mixner has died
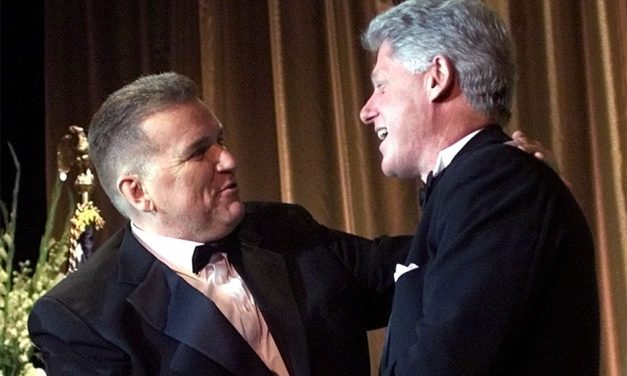
David Mixner, a “founding father” of the LGBTQ+ Victory Fund, a leading LGBTQ activist in the 1980s and ’90s and an advisor to then-candidate Bill Clinton’s presidential campaign has died. He was 77.
Read More